Venous Reflux Disease – Common Cause of Varicose Veins
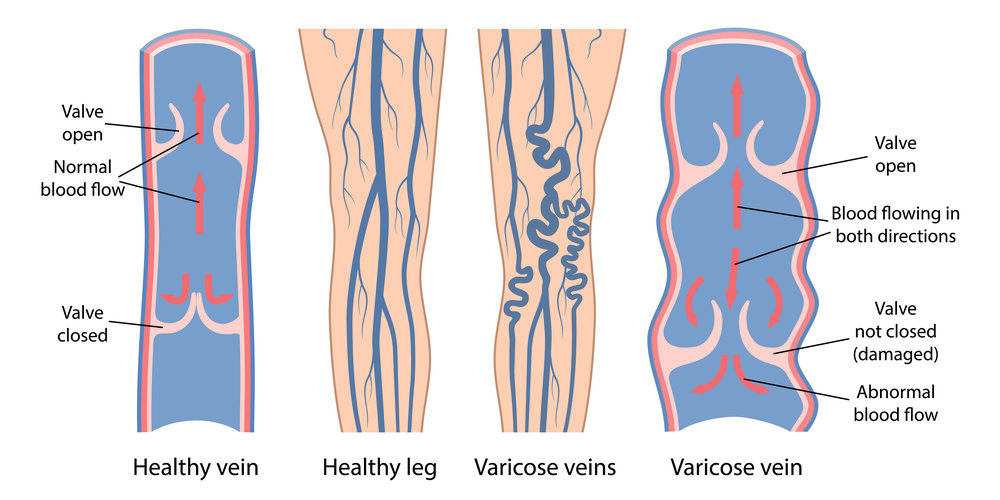
Venous reflux disease is an inherited or acquired disease that affects the valves within the leg’s veins. It leads to the leg vein valves malfunctioning, allowing the abnormal backward flow of venous blood. It is the underlying reason that varicose veins develop in the legs. Venous reflux disease is most commonly inherited or genetically acquired. It, therefore, tends to run in families. It can occasionally occur in the ovarian and pelvic veins (i.e. ovarian vein reflux) but it is much more common in the leg veins. There are some situations in which the disease is acquired as the result of blood clots or trauma damaging the veins and the valves within the veins.
Venous reflux disease is often referred to as chronic venous insufficiency (CVI) or vein valve disease. It is a very common condition, affecting up to 30% of the adult population. This disease is more common in women, with a female to male predominance of three to one. The faulty vein valves lead to a back-up of blood flow, called venous stasis. Normally, healthy vein valves act as a “conveyor belt” to carry blood toward the heart, each valve doing its part to push blood up the leg against gravity. But with venous reflux, the faulty vein valves lose the ability to push blood up the leg, leading to backward blood flow down the leg. This leads to excessive pressure buildup in the legs, known as venous hypertension. It also prevents the de-oxygenated blood of the legs from replenishing itself with oxygen. Over time, the chronic pressure build-up causes the surface vein walls to thin and weaken. Eventually, these weakened veins begin to stretch and bulge out or “balloon out”. The engorged and stretched-out veins appear at the surface of the skin as abnormal veins. The largest of these stretched veins are blue and bulging and are referred to as varicose veins. The smaller diseased veins are referred to as spider veins or reticular veins.
What increases my risk of developing venous reflux disease and varicose veins of the leg?
Genetics is the biggest risk factor. If you inherit the gene for venous reflux disease, you are likely to develop varicose veins of the legs no matter how healthy a lifestyle that you live. So if you have a family member or multiple family members with leg vein problems, you are much more likely to develop varicose veins. Age is also a risk factor. The older you are the more likely you are to develop varicose veins. The most common age to first present to the doctor with varicose veins is age 30-50 years old. But individuals of any age can still develop them. Female gender is a risk factor, likely as a hormonal effect that is poorly understood. Being overweight or living a sedentary lifestyle are also risk factors. Obesity is a particularly high risk, as the extra weight puts significant excess pressure on the leg veins. Pregnancy is a risk factor, as the enlarged uterus also puts excess pressure on the leg veins (more so on the right leg). The more children/pregnancies that a woman has, the higher the risk for developing venous reflux disease. Previous vein injury secondary to phlebitis or previous leg trauma, surgery, or blood clots can also increase your risk of damaging your vein valves and developing venous reflux disease. Environmental or behavioral factors such as occupations in which you are required to do prolonged standing and perhaps a prolonged sitting posture can increase your risks due to the gravity effect on the genetically weak valves.

How is venous reflux disease leading to varicose veins diagnosed?
A special type of venous ultrasound, called a venous reflux ultrasound, is used to diagnose this condition. This study should always be performed while the patient is in the STANDING position, as it is not accurate when performed lying down. It should also be performed at a vein center by an RVT or RPVI that has experience with venous reflux ultrasound testing. This type of ultrasound testing takes particular expertise and experience to be performed correctly. Therefore, the ultrasound should always be performed by individuals with the proper level of training and experience. It has been our experience that vein centers that are run by RPVI physicians and vascular specialists tend to have the most accurate vein ultrasound results due to the experience and qualifications of the individuals performing and interpreting the exams. When it comes to pelvic varicose veins, a different type of study known as a catheter venogram or magnetic resonance venogram may be necessary to appropriately diagnose pelvic congestion syndrome / pelvic venous incompetence.

What kind of problems can you develop if you have venous reflux disease of the legs?
Venous reflux disease of the legs is almost always a progressive disease and typically worsens the longer you have the condition. So the earlier in life that you develop the disease the more problems you will typically develop. There are a large variety of problems that can develop in the legs, ankles, and feet as a result of the disease.
These problems are listed below:
- Varicose veins of the legs or ankles
- Leg pain or chronic leg discomfort
- Leg swelling
- Spider veins and reticular veins of the legs or feet
- Skin discoloration leads to darkening of the skin of the lower legs that are often brown or tan in color
- Skin wounds of skin ulcers of the ankles or feet
- Bleeding from skin veins
- Blood clots or vein thrombosis
- Venous stasis ulceration
- Skin damage that can lead to hardening of the skin or skin rashes
- Numbness or tingling of the legs or feet
- Restless leg syndrome
- Peripheral neuropathy
How is venous reflux disease treated?
There are several methods used to treat venous reflux disease leading to varicose veins of the legs. The particular anatomy of the venous disease condition while dictating which method of treatment will be best.
The various methods of treatment are briefly described below:
- EndoVenous Laser Therapy, known as EVLT or EVLA, uses laser energy to treat venous reflux disease and varicose veins of the legs.
- Radiofrequency vein ablation, known as RF ablation, Venefit procedure, or VNUS closure treatment used radiofrequency energy to treat venous reflux disease and varicose veins of the legs.
- Ultrasound-guided foam sclerotherapy uses endovenous chemical ablation to treat varicose veins and venous reflux disease of the legs and pelvis. Varithena is a common medication utilized for this therapy.
- Vein surgery, known as phlebectomy or vein stripping, can be used to treat venous reflux disease and varicose veins of the legs.
- ClariVein® is a specialty vein infusion catheter with a rotating tip that promotes controlled drug coverage of targeted treatment areas of the legs to treat venous reflux disease and varicose vein. It uses a combination of chemical and mechanical ablation to treat defective leg veins.
- VenaSeal, a medical glue designed for leg veins, is another very effective therapy.
Can venous reflux disease and varicose veins be cured?
Yes, often venous reflux disease and be cured through treatments by a vein specialist. By treating and curing the vein disease it will prevent you from developing further problems in your legs in the future. Our vein specialists can discuss your individual situation after they do an examination of your legs.
To learn more about venous reflux disease and varicose veins, please contact Austin Vein Specialists at (512) 220-5401. We offer a no-obligation consultation with one of our top rated and board-certified physicians.
- Varicose veins of the legs or ankles
- Leg pain or chronic leg discomfort
- Leg swelling
- Spider veins and reticular veins of the legs or feet
- Skin discoloration leads to darkening of the skin of the lower legs that are often brown or tan in color
- Skin wounds of skin ulcers of the ankles or feet
- Bleeding from skin veins
- Blood clots or vein thrombosis
- Venous stasis ulceration
- Skin damage that can lead to hardening of the skin or skin rashes
- Numbness or tingling of the legs or feet
- Restless leg syndrome
- Peripheral neuropathy